Can proteins help in managing type II diabetes?
Type II diabetes (T2D) is a disease characterized by high blood glucose called hyperglycemia. Healthful eating, physical activity and pharmacotherapy (in many cases) are considered as the foundation for diabetes management[1]. It is well known that nutrition and meal planning for T2D patients are the most challenging in diabetes self-care[2]. In addition, more and more evidence about the positive physiologic function of dietary proteins, part of overall diet, for Type II Diabetes and prediabetes management are demonstrated[3].
What is type II diabetes?
Generally, Type II Diabetes is characterized by insulin resistance, meaning that body (mostly muscle and liver – glucose storage into glycogen form) is not capable to respond to insulin, which plays a regulatory role by keeping blood sugar at normal values. As a consequence, blood glucose is less stored, its level keep rising and more insulin is secreted by the pancreas. To a certain point, the latter produces less and less insulin resulting on higher blood sugar levels (Figure 1).
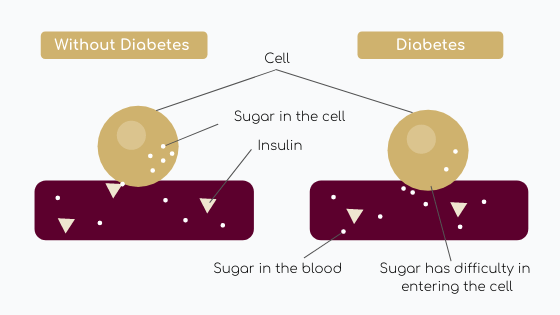 Figure 1: Diabete physiopathology diagram
Figure 1: Diabete physiopathology diagram
According to World Health Organization (WHO), fasting plasma glucose values upper 126 mg/dl with signs and symptoms is one of diabetes diagnosis[4]. Older adults are mostly touched by T2D even if we observed more and more children, adolescents and younger adults with this disease[5]. This increase prevalence in younger people might be due to higher obesity level, less physical activity and poor diet[5].
Incidence and prevalence of type I & type II diabetes – difference by geographical areas:
The International Diabetes Federation (IDF) has predicted that people number with diabetes (Type 1 & 2) is anticipated to rise from 425 million in 2017 to 629 million by 2045 in adults[6]. Globally, prevalence is estimated to increase from 8.3% in 2019 to 9.6% in 2045 (Figure 2)[6].
Otherwise, disparities do exist between world regions. On one hand, diabetes prevalence in Middle East and North Africa (MENA) Region presents the highest age-adjusted prevalence of diabetes in adults[6]. On the other hand, Africa region presents the lowest age-adjusted prevalence (Figure 1)[6]
Concerning number of cases, countries with the highest number of diabetes people are China, India and United States of America, and are projected to persist so until 2030[6].
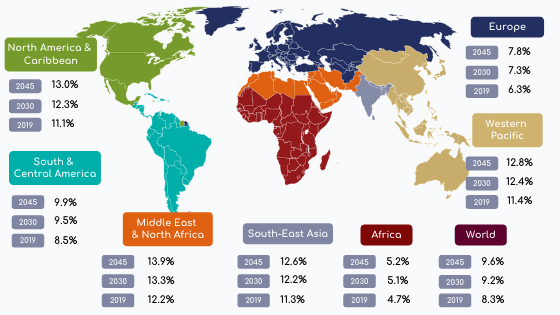
Figure 2: Prevalence of diabetes in adults (20-79 years) in the world (Adapted from IDF.org [6])
90% of diabetes is represented by T2D[5]. Why such increase in people living with T2D?
It might be explained by changes in diet and reduced physical activity related to urbanization.
TD2 risks and factors
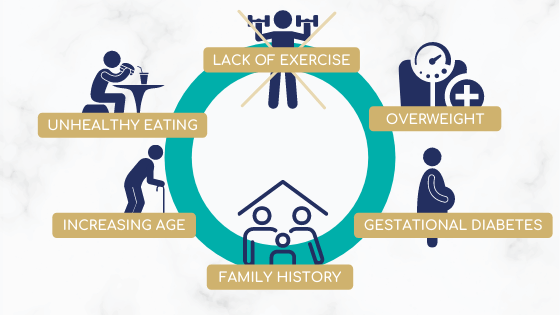
Figure 3: Examples of T2D risk factors (Adapted from IDF.org[5])
Type II diabetes symptoms
Several symptoms are encountered in Type II Diabetes patients[5].
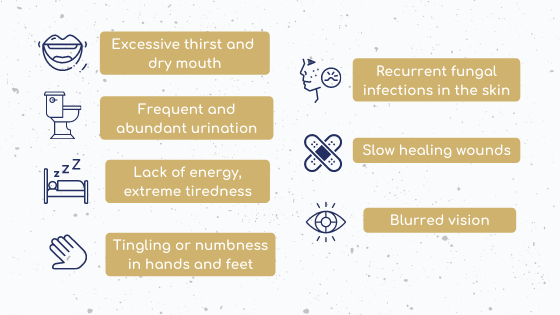
Figure 4: Symptoms of T2D (Adapted from IDF.org[5])
Social economic Impact
Annual global health is estimated at USD 760 billion by IDF[7]. This cost is projected to increase and might reach USD 825 billion by 2030 and 845 billion by 2045[7]. Health complication of Diabetes, as premature death or disability, are associated with a negative economic impact and add 35% to the annual global health expenditure[7].
Milk protein roles in diabetes management
Diabetes dietary recommendations
Type II Diabetes management is composed by healthy diet recommendations, increasing physical activity and healthy body weight maintenance. To help blood glucose levels control, oral medication and insulin injection are frequently prescribed[5].
We know that insulin resistance is a key component in the progression of T2D. In addition, high body weight is a predominant factor in insulin resistance development[8]. Indeed, interventions demonstrated that insulin sensitivity and diabetes control are improved with 7-10% weight loss in T2D patients[9]. As a result, International Diabetes Federation recommends that T2D overweight and obese patients should reduce daily caloric (-500 to 600 Kcal). They also recommend to avoid sugar, sweets and sweetened beverages and to prefer high fiber and low-glycemic index foods[10].
What about proteins?
Proteins play an essential role for the human body. Indeed, they are used to repair, build and renew body tissues as skin, hair, nails, muscles, etc. Contrary to misconception, protein does not induce hyperglycemia[3]. Today, there is no global consensus to recommend a protein intake for glycaemia optimization1 but foundations, as American Diabetes Association, proposed the following recommendation: Diabetic patients without chronic kidney disease should have a protein intake greater than 1g/kg[11]. For example, diabetic patients need a protein intake of 70g for people weighing 70kg.
Which source is the best?
The best source of protein for diabetes dietary management is still under investigation even if several prospective cohort suggested differences between T2D outcomes and protein source[12]. An inverse association between dairy protein intakes and T2D risk has been observed by several prospective cohort studies[13]. Today, this potential protective mechanism of dairies is not fully understood. Moreover, randomized controlled trials is limited and do not permit to recommend a certain source of protein[3].
What about whey protein? How does it work?
The “Whey” to lower glycaemia
A right protein intake could be beneficial by helping in satiety, preservation of lean body mass[14] (eg muscles) during weight loss. Concerning glycemic control, whey protein seems to impact post prandial glycaemia via insulin ways[15]. Indeed, it seems that whey protein, a rich source of amino acids, enhances insulin secretion[16,17]. Among these amino acids, Leucine is of interest because it exerts effects on pancreatic β-cells, liver, muscle and adipose tissue and so recognized as a glucose homeostasis influencer[18]. In a short term clinical study in T2D patients, 50g whey protein consumption prior to high Glycemic Index Breakfast decreased postprandial glycaemia[19]
Indeed, it seems that whey protein, a rich source of amino acids, enhances insulin secretion.
Is it the only explanation? The whey might has an impact on glycaemia through gastric emptying modulation in healthy[20] and diabetic[21] population. Indeed, by slowing it, it can decrease post prandial glucose liberation[22,23].
Concerning whey supplementation long-term effects, the number of studies is very low and limited data were published concerning its impact on glycemic control. For example, in T2D patients, one study showed that 25g of whey protein during 4 weeks slowed gastric emptying and reduce postprandial glycaemia in preload[24]. The same has been observed recently with 17g of Whey associate to guar during 12 weeks[25].
To conclude, a right protein intake could be beneficial by preservation of lean body mass during weight loss. Concerning whey, it seems to impact post prandial glycaemia via insulin ways[15] or by slowing gastric emptying and so glucose liberation[22,23].
Our Pronativ® native whey proteins is particularly rich in leucine and regarding bibliographical data, therefore might enter into dietary management of diabetes by helping in normalization of glucose homeostasis.
Sources
1. Evert, A. B. et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 36, 3821–3842 (2013).
2. Yancy, W. S., Foy, M., Chalecki, A. M., Vernon, M. C. & Westman, E. C. A low-carbohydrate, ketogenic diet to treat type 2 diabetes. Nutr. Metab. 2, 34 (2005).
3. Campbell, A. P. & Rains, T. M. Dietary protein is important in the practical management of prediabetes and type 2 diabetes. J. Nutr. 145, 164S-169S (2015).
4. World Health Organization & International Diabetes Federation. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: report of a WHO/IDF consultation. (2006).
5. Type 2 diabetes. https://idf.org/aboutdiabetes/type-2-diabetes.html.
6. Demographic and geographic outline. https://diabetesatlas.org/en/sections/demographic-and-geographic-outline.html.
7. Individual, social and economic impact. https://diabetesatlas.org/en/sections/individual-social-and-economic-impact.html.
8. Chiasson, J.-L. & Rabasa-Lhoret, R. Prevention of type 2 diabetes: insulin resistance and beta-cell function. Diabetes 53 Suppl 3, S34-38 (2004).
9. Look AHEAD Research Group et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care 30, 1374–1383 (2007).
10. Guidelines. https://idf.org/e-library/guidelines/128-idf-clinical-practice-recommendations-for-managing-type-2-diabetes-in-primary-care.html.
11. Hamdy, O. & Horton, E. S. Protein Content in Diabetes Nutrition Plan. Curr. Diab. Rep. 11, 111–119 (2011).
12. Sluijs, I. et al. Dietary intake of total, animal, and vegetable protein and risk of type 2 diabetes in the European Prospective Investigation into Cancer and Nutrition (EPIC)-NL study. Diabetes Care 33, 43–48 (2010).
13. Hirahatake, K. M., Slavin, J. L., Maki, K. C. & Adams, S. H. Associations between dairy foods, diabetes, and metabolic health: potential mechanisms and future directions. Metabolism. 63, 618–627 (2014).
14. Martens, E. A. P. & Westerterp-Plantenga, M. S. Protein diets, body weight loss and weight maintenance. Curr. Opin. Clin. Nutr. Metab. Care 17, 75–79 (2014).
15. Akhavan, T. et al. Mechanism of action of pre-meal consumption of whey protein on glycemic control in young adults. J. Nutr. Biochem. 25, 36–43 (2014).
16. Floyd, J. C., Fajans, S. S., Conn, J. W., Knopf, R. F. & Rull, J. Stimulation of insulin secretion by amino acids. J. Clin. Invest. 45, 1487–1502 (1966).
17. Floyd, J. C. et al. Synergistic effect of essential amino acids and glucose upon insulin secretion in man. Diabetes 19, 109–115 (1970).
18. Yang, J., Chi, Y., Burkhardt, B. R., Guan, Y. & Wolf, B. A. Leucine metabolism in regulation of insulin secretion from pancreatic beta cells. Nutr. Rev. 68, 270–279 (2010).
19. Jakubowicz, D. et al. Incretin, insulinotropic and glucose-lowering effects of whey protein pre-load in type 2 diabetes: a randomised clinical trial. Diabetologia 57, 1807–1811 (2014).
20. Akhavan, T., Luhovyy, B. L., Brown, P. H., Cho, C. E. & Anderson, G. H. Effect of premeal consumption of whey protein and its hydrolysate on food intake and postmeal glycemia and insulin responses in young adults. Am. J. Clin. Nutr. 91, 966–975 (2010).
21. Ma, J. et al. Effects of a protein preload on gastric emptying, glycemia, and gut hormones after a carbohydrate meal in diet-controlled type 2 diabetes. Diabetes Care 32, 1600–1602 (2009).
22. Horowitz, M., Edelbroek, M. A., Wishart, J. M. & Straathof, J. W. Relationship between oral glucose tolerance and gastric emptying in normal healthy subjects. Diabetologia 36, 857–862 (1993).
23. Marathe, C. S., Rayner, C. K., Jones, K. L. & Horowitz, M. Relationships between gastric emptying, postprandial glycemia, and incretin hormones. Diabetes Care 36, 1396–1405 (2013).
24. Ma, J. et al. Sustained effects of a protein ‘preload’ on glycaemia and gastric emptying over 4 weeks in patients with type 2 diabetes: A randomized clinical trial. Diabetes Res. Clin. Pract. 108, e31-34 (2015).
25. Watson, L. E. et al. A whey/guar ‘preload’ improves postprandial glycaemia and glycated haemoglobin levels in type 2 diabetes: A 12-week, single-blind, randomized, placebo-controlled trial. Diabetes Obes. Metab. 21, 930–938 (2019).